Dr. Hall
I had tooth #17 (lower left wisdom tooth) extracted about 6 weeks ago. I wanted to see it after the dentist took it out, but he wouldn’t let me touch it or have it. The gum took about 3 weeks to fully close back up. I started having pain on the left side of my face, in my ear and in the back of my left eye. The pain has subsided but not in the back of my eye. I’m suspicious that my dentist was trying to hide the tooth from me because he didn’t get all of it out. Could the pain I continue to have be because of an infection from a piece of the tooth being left behind?
– Leslie from the Bahamas
(See Dr. Hall’s answer below.)
We thank our advertisers who help fund this site.
Leslie,
It does sound suspicious. It is possible to have a post-operative infection after taking out a wisdom tooth, but that generally only happens in the case of an impaction where the gum is sutured closed again after the surgery. When the tooth wasn’t impacted and there is an open socket, which is what you are hinting happened with you, any infection will drain out through the opening and it should heal without complication.
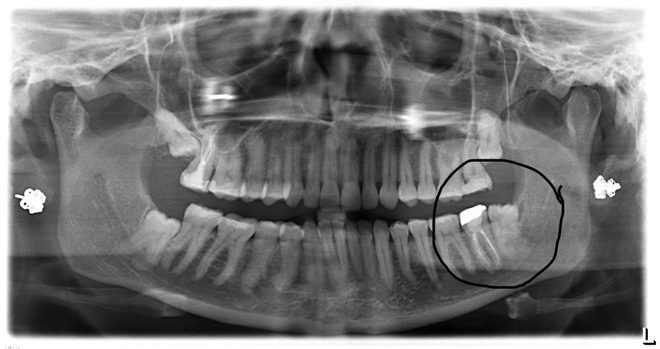
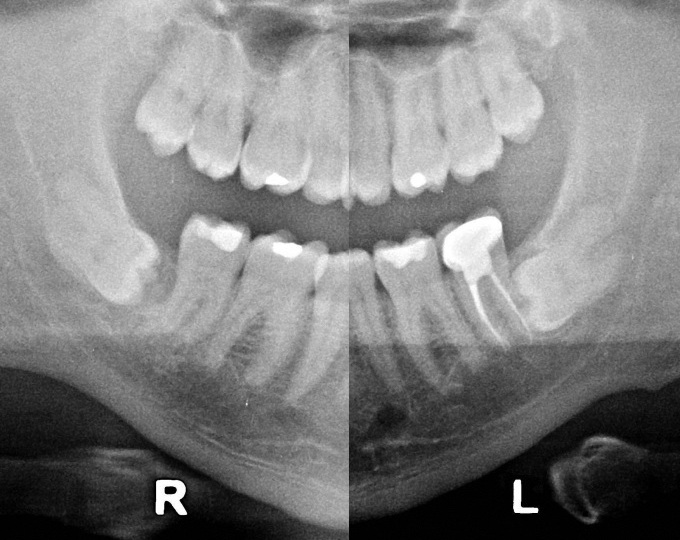
But if a significant piece of the tooth were left in the socket, such as entire root, yes, the gum could heal over it, leaving this root embedded in your jaw and susceptible to a post-operative infection.
I would find another dentist and have them take an x-ray of your wisdom tooth area to see if this is the case. It would be best to go to an oral surgeon who could handle finishing the extraction if that turns out to be necessary. If there is still a root there and the bone hasn’t healed over it, you could have the root removed without a lot of trouble. If there is a root that was left, I would be inclined to ask for a refund from your dentist.
What Should a Dentist Do When a Tooth Breaks During an Extraction
Unforeseen complications can easily happen during an extraction. Especially in older patients, sometimes roots will have extra cementum deposited so that the end of the root is fatter, which can cause the root to break off when the tooth is extracted. I wouldn’t blame the dentist for this.
If it’s just a small root tip that breaks off, it can be best just to leave it. If the root tip is near a nerve or close to the sinus, it can be risky to go after it. But the dentist should tell you when this happens. And it should heal with no complications.
If a large piece of the root breaks off, it should be removed. Doing so will generally require removing some bone around the root. If the dentist has the skills to do that, he or she can complete the extraction. If they don’t, they should refer you to an oral surgeon to complete the procedure. In either case, you should be informed of the complication.
Also, it isn’t uncommon for a patient to want to take the extracted tooth home and some dentists will routinely give that to the patient. If you asked and he didn’t let you see it, yes, I would be suspicious.
– Dr. Hall
Do you have a comment or anything else to add? We’d love to hear from you. Enter your comment below. Or click here to ask Dr. Hall a question.
About David A. Hall
Dr. David A. Hall was one of the first 40 accredited cosmetic dentists in the world. He practiced cosmetic dentistry in Iowa, and in 1990 earned his accreditation with the American Academy of Cosmetic Dentistry. He is now president of Infinity Dental Web, a company in Mesa, Arizona that does advanced internet marketing for dentists.