Hello Dr. Hall,
I had a root canal on my upper right canine. The temporary filling came out and an abscess developed on my gum. I returned to my dentist’s office. He said I needed a second root canal to address the abscess. The abscess is not painful unless I press on the affected area. Is the abscess “toxic” and would antibiotics work or just the 2nd root canal?
Thank you for your attention,
-Mark Mesi
(See Dr. Hall’s answer below.)
We thank our advertisers who help fund this site.
Mark,
Yes, you absolutely need to have this root canal treatment re-done.
Let me start by explaining what I believe happened. I’m going to read between the lines here since you didn’t give me all the details. You said the temporary filling came out. I want to explain why this causes a problem.
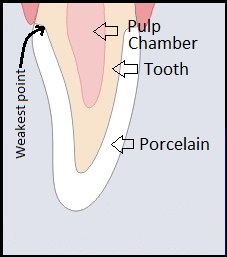
When a dentist does a root canal treatment on an infected tooth, the infection is cleaned out of the inside of the tooth and the root is then sealed with a filling material and cement. The seal needs to be protected or bacteria will get back into the tooth and the infection will return. To protect the tooth, a temporary filling will be placed at the end of your root canal appointment. If the root canal filling isn’t protected from saliva, it won’t take long for the saliva to seep into the filling and break the seal. So the temporary filling is placed and you should then be scheduled for final restoration of the tooth—usually a crown, or sometimes just a filling may do.
So it looks like someone didn’t follow through here and the temporary filling, being just temporary, came out. These temporary fillings are purposely made so that they are very easy to take out. Now your root canal treatment was exposed to saliva. Over a period of several days, the saliva will break down the seal of the root canal and the infection will return.
About the Antibiotics
You asked if you could just treat this with antibiotics and avoid re-treatment. Here’s why that won’t work. When you take antibiotics, they get into your bloodstream to fight the infection. However, there is no blood circulation inside your tooth, so antibiotics cannot get there to remove the infection. They can temporarily eliminate the abscess in your gum and bone, but as soon as you stop taking them the abscess will return. To complicate things, by taking the antibiotics you will be helping breed antibiotic-resistant bacteria, which is a very risky thing.
Since this doesn’t hurt, can you just leave it alone? Infections in your jawbone, particularly in the upper jaw, are risky in that they can spread to your eye or your brain. I wouldn’t mess with that. There is a famous story of a boy in Maryland who died from a tooth infection about 15 years ago.
Furthermore, with oral bacteria having an undisturbed existence inside your tooth, decay will begin to grow there from the inside out and, in time, your tooth will be unrestorable.
Just get it fixed.
– Dr. Hall
Do you have a comment or anything else to add? We’d love to hear from you. Enter your comment below. Or click here to ask Dr. Hall a question.
About David A. Hall
Dr. David A. Hall was one of the first 40 accredited cosmetic dentists in the world. He practiced cosmetic dentistry in Iowa, and in 1990 earned his accreditation with the American Academy of Cosmetic Dentistry. He is now president of Infinity Dental Web, a company in Mesa, Arizona that does advanced internet marketing for dentists.